In 2020, headlines were made globally after a study involving almost 55,000 subjects from the EPIC-Oxford cohort was published. These headlines suggested that adopting a vegan diet could result in weak bones that are more susceptible to fracture.1 Is this cause for concern? Are vegans really at a greater risk of bone fracture? Let’s take a deeper look at the study and determine together what we can make of it.
The first thing to understand about this study is who the subjects are. The EPIC-Oxford cohort is a group of British subjects recruited between 1993 and 2001 who have been followed since. We therefore have about 2-3 decades of data from a group of people who are now mostly aged in their 60’s. The study included meat-eaters, pescetarians, vegetarians and vegans – allowing the researchers to see if health outcomes differed over time based on the type of diet these individuals were consuming. For example, one of such outcomes the researchers set out to investigate was whether dietary patterns affect bone fracture risk. These studies are called epidemiological and are an important part of the nutrition science puzzle because they help us look at the way our food choices affect our health in ways that short term randomised controlled trials (RCTs) cannot.
Before we get into the study results, there are a few other characteristics of this study that are worth noting. For starters, the vegan portion of the cohort consumed on average 26g of fibre per day. While this was certainly higher than the other dietary groups in the study, it is much lower than we would expect for vegans eating a healthy, whole-food based diet. For example, in a 2017 study of omnivores, vegetarians and vegans from Switzerland, vegans averaged 52g of fibre per day.2 Based on this, we can assume that the vegan diet adopted by those in the EPIC-Oxford cohort was probably not on par with the diet that many health-conscious vegans, who are following a more whole-food plant-based diet, are eating today. This could be explained by the fact that in the 1990’s and early 2000’s there was considerably less nutritional information available for people adopting a vegan diet. It may also be that many of the vegan subjects were adopting a vegan diet for ethical reasons, and were not overly concerned about planning their diet with optimal health outcomes in mind. The fact that only 51% of the vegan subjects took a supplement is further evidence of this – today it is very much well known that all vegans should supplement with Vitamin B12 as a bare minimum.3
In addition to what appears to be a rather average vegan diet with little to no supplementation , previous studies of the EPIC-Oxford study were able to identify that vegans were more likely to be vitamin D deficient in winter. 3 Indeed, while most vitamin D comes from exposure to the sun, around 20% of vitamin D in the average omnivore diet comes from animal foods. Therefore, it makes sense that vegans who are not supplementing and are from northern latitudes would be at greater risk of developing vitamin D deficiency. This is important to note because we know vitamin D plays a crucial role in building and maintaining healthy bones, and studies have shown when vegans supplement with Vitamin D (as recommended in Simon’s book The Proof is in the Plants), even with very low dosages, their bone mineral density improves.
So, what exactly did the study show? The EPIC-Oxford study specifically identified that over a 10-year period, vegans experienced 20 more broken bones for every 1000 people. Put simply, that means if you compared 1000 vegans with 1000 omnivores in this cohort, there were 20 more fractures in the vegan group over the 10 years. This risk was only observed in post-menopausal women and people with a lower BMI. Importantly, the researchers concluded that even when calcium and protein were controlled for (e.g comparing meat-eaters and vegans who consumed similar amounts of protein and calcium), two nutrients known to affect bone health, vegans were still at a higher risk of developing bone fractures. Taken at face value, this finding seemed to infer that vegan diets are inherently bad for bone health. However, before we throw the baby out with the bathwater, there are a few elements to this study that are worth paying attention to.
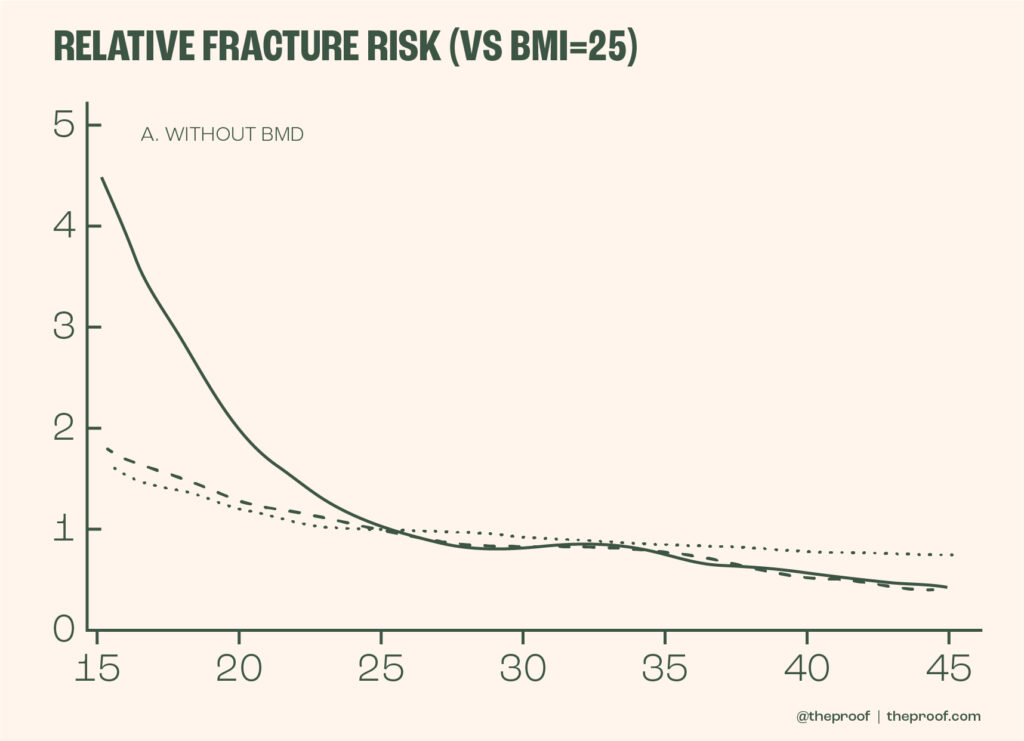
The first is how the researchers controlled for body weight. We know from large amounts of data that a low body weight increases one’s risk of fracture.4,5 Carrying less weight means less force through our bones (resistance promotes greater bone density) and as well as a reduced amount of cushioning if one experiences a fall – which is not an ideal combination. If we want to see whether a vegan diet is inherently bad for bone health, then ideally we want to compare vegans and meat-eaters that are the same weight. That way, we reduce any signal or noise that would likely exist simply as a result of the fact that vegans tend to have a much lower BMI. Now, to the researcher’s credit, they did attempt this, but they made a rather large error.In fact, rather than using a statistical model that allowed for people to be compared at specific BMI levels (e.g comparing omnivores and vegans with the exact same BMI), they simply compared people within a BMI range (e.g. everyone with a BMI under 18.5, comparing all vegans and meat-eaters with a BMI under this point). The problem here is that, as you can see on the risk curve below, the risk from 18.5 down to 15 essentially doubles from a relative risk of around 2.2 to over 4. The fact that more vegans in the <18.5 BMI group were likely to be nearer to 15, likely explains most of the higher fracture risk observed. This is well summarised in Dr Avi Bittman’s video analysis here.
The take home point here is that because of the chosen statistical model, there is a high possibility that the increased risk in fracture is greatly influenced by the simple fact that there were more vegans at the lower end of the BMI range. This is not an inherent problem with vegan food, but more so speaks to the importance for vegans to ensure they eat enough calories and maintain a healthy body weight and do not become too light.
Image 1 – Risk of fracture at different BMI levels 4
So, what’s the takeaway point here? This study provides no plausible reason to believe that a vegan diet is inherently bad for bone health. Rather, it just reiterates what we already know about building strong bones – it’s a team effort and a holistic approach is required. Aside from maintaining a healthy body weight, it is a good idea for anyone following a whole-food plant based diet to:
- Consume adequate amounts of calcium (>700 mg per day)6. This is the RDI in the UK and is consistent with a large study from Sweden involving over 60,000 women who were followed for 19 years.6 Around 700 mg of calcium per day saw the lowest risk of fracture, with no greater reduction in risk at levels above this. In fact, if anything, there was a trend towards increased risk of fracture as calcium went above this level. While adequate amounts of calcium can be consumed from whole plant foods, the addition of fortified foods can be helpful (e.g plant-based milk). The vegans in this EPIC-Oxford study only averaged 591 mg of calcium per day. Whereas, other vegan cohorts have been shown to average 800-1000 mg per day.
- Ensure healthy vitamin D status all year
- Supplement with vitamin B12
- Perform regular resistance exercise (body weight or with weights/bands etc)
- Consume 3+ serves of legumes per day to ensure adequate protein intake (As one gets towards 65 years of age I recommend increasing this to 4+ serves a day as protein requirements slightly increase in our later years to help prevent muscle wasting which is very much correlated with increased risk of premature death)
For more information on bone health, calcium and other nutrients of focus for those following a plant-predominant or plant-exclusive diet, please grab a copy of The Proof is in the Plants. When you purchase this book you will also gain access to the below bonus e-guides:
- Supplement guide (most bioavailable forms, dosages and the brands I recommend)
- Blood test guide (with specifics on why the B12 test commonly ordered is not very reliable)
- Tracking your progress guide
- Plant Proof Food and Oil Pyramid guide
References:
2. Schüpbach R, E. al. Micronutrient status and intake in omnivores, vegetarians and vegans in Switzerland. – PubMed – NCBI. https://www.ncbi.nlm.nih.gov/pubmed/26502280.
5. Are Vegans at Higher Risk for Bone Fractures? Debunking the EPIC-Oxford study. (2020).